What is it?

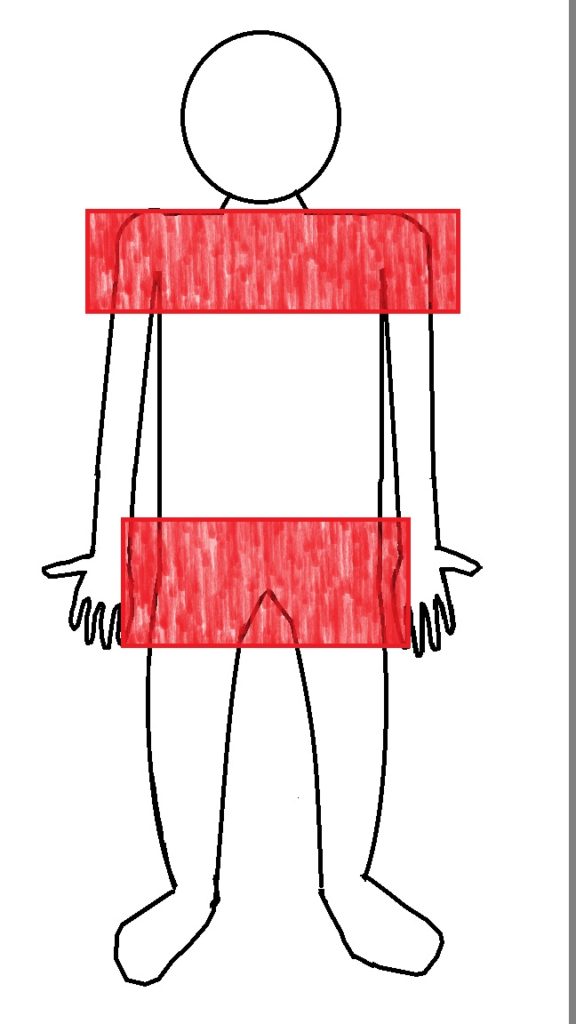
Polymyalgia Rheumatica (PMR) is a relatively common inflammatory condition that causes aching pain and stiffness in the shoulders, hips, neck, and back. The term “polymyalgia” means many muscle pains.
Who gets it?
There are certain risk factors that make PMR more likely
Age:
– This condition is almost only seen in people over the age of 50
– The Incidence of the condition increases with age
– The peak incidence is around 70 – 80 years of age
Gender:
– Women are affected more than men (about 2-3 times more)
Ethnicity:
– People of Scandinavian and Northern European decent have a higher incidence of the condition
Genetics:
– The condition is associated with the HLA-DR4 haplotype
– A high level of IL-6 (a pro-inflammatory cytokine) has also been associated with this condition
What exactly happens in the disease?
The exact cause of the PMR is unknown, though it is believed to have a genetic factor to it. Environmental and infectious causes were studied, but have been inconclusive.
What are the symptoms?
Patients with this condition usually have symmetrical pain in the shoulders, hips, neck, back, and torso, described as an aching pain and stiffness. It has been shown that not only are the joints involved, but the bursa around the joints, making the pain in the arms and thighs a “referred pain”. The pain is usually abrupt onset, worse in the morning (with morning stiffness lasting > 1 hour), and usually limits normal daily activity, even simple activities such as putting on a shirt, getting to a standing position, and going up stairs, putting on shows or socks. The pain usually starts in the shoulders, and can be on one side, but usually becomes bilateral in a few weeks. Stiffness can occur after prolonged times of rest, known as the “gel phenomenon”. Patient can also have distal arthritis and even edema (swelling of the extremities)
Systemic findings include:
– Weight loss
– Low-grade fevers
– Fatigue
– Malaise
– Depression
– Difficulty getting out of bed, out of a chair, or off the toilet
– Difficulty with daily activities (dressing, bathing, etc.)
Musculoskeletal findings include:
– Morning stiffness > 1 hour
– Muscle stiffness after prolonged inactivity (“gel phenomenon”)
– Arthritis in the distal joints (hands, feet, etc.)
– Joint swelling, particularly in the affected joints
– Carpal tunnel syndrome
– Swelling of the hands and feet
– Patients can also suffer from fatigue, decreased appetite, and sometimes low grade fevers.
In some cases (around 10% of patients with PMR), patients may experience a related condition known as Giant Cell (Temporal) Arteritis, also called GCA, in which patient get inflamed blood vessels and present with high fevers, headaches, blurry vision, and jaw complaints (GCA discussed here)
How is it diagnosed?
Unfortunately, there is not a specific test for PMR. The diagnosis is made based on the history, risk factors, symptoms, examination, and blood work. Blood work tends to show elevation in the markers of inflammation, specifically the Erythrocyte Sedimentation Rate (ESR) and the C – reactive protein (CRP). Though these labs are not specific, they are often elevated in PMR (though can be low in some cases). Imaging studies are usually not done as they tend to be unrevealing. MRI has been used before, and usually shows synovitis (inflammation) in the affected joints as well as bursitis. These findings are not specific, and hence why MRI is usually not used.
How is it treated?
The good news is that most cases are treated successfully with oral steroids (prednisone), and most patients notice an improvement within a few days. The bad news is that most patients must stay on prednisone for a prolonged period of time (anywhere from 6 months to 2 years +) as it is taper off slowly to prevent relapse. For more resistant cases or development of GCA, patients may need higher doses of steroids or the addition of stronger anti-inflammatory medications, such as Methotrexate or Tocilizumab. NSAIDs (Ibuprofen, Naproxen, etc.) can help with some of the pain, but do not address the underlying cause of symptoms. Physical therapy can help maintain activity, but again, will not resolve the underlying cause.
See Also
Giant Cell (Temporal) Arteritis
References
https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-polymyalgia-rheumatica?source=search_result&search=polymyalgia+rheumatica&selectedTitle=1%7E84
https://www.mayoclinic.org/diseases-conditions/polymyalgia-rheumatica/symptoms-causes/syc-20376539
https://emedicine.medscape.com/article/330815-workup
https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Polymyalgia-Rheumatica






