Although classic gout- ie. gout appearing as a painful, swollen, and red big toe- is easily recognized by most people, gout does not always present in this fashion. Similarly, treatment of gout may seem straight forward at first, but there are so many details to consider depending on the individual, their co-morbidities, and the way their gout behaves. Therefore, gout diagnosis and treatment often require an expert’s touch!
Diagnosing gout
Gout is suspected when someone has acute onset of a red, hot, swollen and tender joint. If the affected joint is a great toe, the suspicion is even stronger. Blood tests may show an elevated uric acid level which would be expected with gout. Xrays may be normal or may show evidence of joint destruction from tophi.
Although at times the clinical picture is all the information we have to make the diagnosis, relying on the uric acid levels alone may be misleading. Uric acid levels may be spuriously low during an attack, giving us a false negative. Also, most people with an elevated uric acid may not have gout, so there is a high chance of false positives. Other types of arthritis, including infection of a joint, can also look like gout clinically.
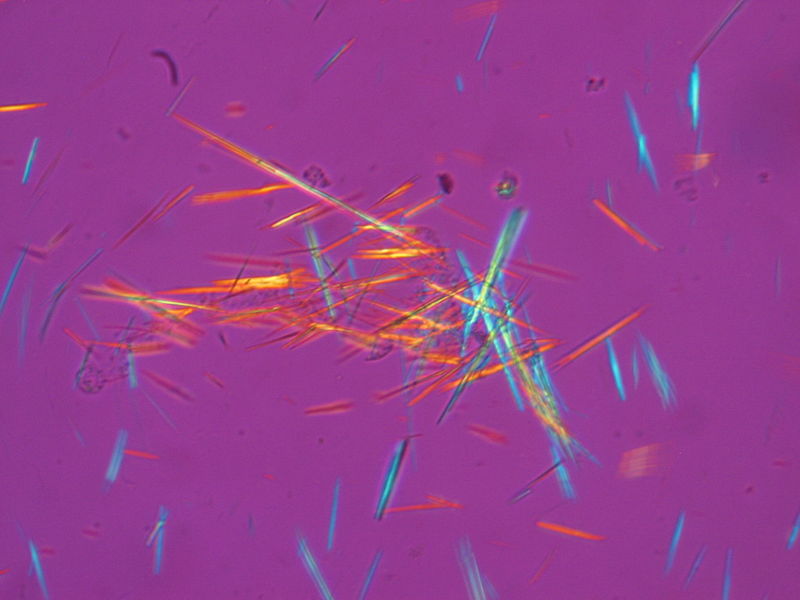
The gold standard of gout diagnosis is presence of monosodium urate crystals in the fluid from a joint. These crystals are needle-shaped structures that look either blue or red- depending on their orientation- under a polarized microscope. To find these crystals, a sample of the fluid is removed from the joint with a needle and looked at under the microscope.
How is gout treated?
Acute gout
The goal in treatment of an acute gout attack is to relieve symptoms quickly. Some of the ways this is achieved are:
- Non-steroidal anti-inflammatory drugs (NSAIDs)– example: ibuprofen (advil), indomethacin (Indocin), Naproxen (Naprosyn), etc.
- Colchicine (Colcrys)
- Steroids – example: prednisone
- Pain medications like vicodin
- Cold packs
NSAIDs should be used with caution in people with kidney disease, heart disease, history of gastric ulcers, and cannot be used in people who take blood thinners. Colchicine should be used carefully in people with kidney disease. Steroids can elevate blood sugar so people with diabetes will need to be monitored on this medication.
Large doses of colchicine can cause diarrhea. In the past, people with acute gout were instructed to take a tablet of colchicine every hour until they developed diarrhea. The new recommendations are to take about two tablets per day, which seems to be just as effective as the higher dose with much less side effects.
Chronic gout
If gout attacks become chronic, long-term medications are used to lower uric acid and prevent future attacks. These include:
- Probenacid– increases uric acid filtration through the kidneys
- Allopurinol– prevents formation of uric acid in the blood
- Febuxostat (Uloric)– similar to Allopurinol, but can be used more safely in people with poor kidney function
- Colchicine (Colcrys)– Low dose colchicine can also be used long term as a prophylaxis drug for gout. Many rheumatologist will combine colchicine with the other long term drugs for the first few months to prevent gout flares as the uric acid level is lowered.
- Pegloticase (Krystexxa)- breaks down uric acid into a product that is more easily eliminated. Since this IV drug can potentially cause severe allergic reactions, it is reserved for very severe cases of gout not otherwise controlled.
Gout prevention
Diet and lifestyle changes can have a large impact on management of gout. See:
Reference:
PubMed Health http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001459/
Wikipedia http://en.wikipedia.org/wiki/Gout






