How is it diagnosed?
Ankylosing spondylitis is diagnosed starting with a thorough history, asking about symptoms and risk factors discussed in previous sections. A detailed exam is necessary to find any kind of inflammatory back signs, peripheral arthritis, or extra-articular manifestations. Certain maneuvers and measurements should be performed in the office. Below are just a few exam techniques that may be used to diagnose AS, such as:
- Occiput-to-wall test: to measure the cervical spine range of motion
- Chest expansion test: to measure the thoracic spine range of motion
- Schober test: to measure lumbar spine range of motion
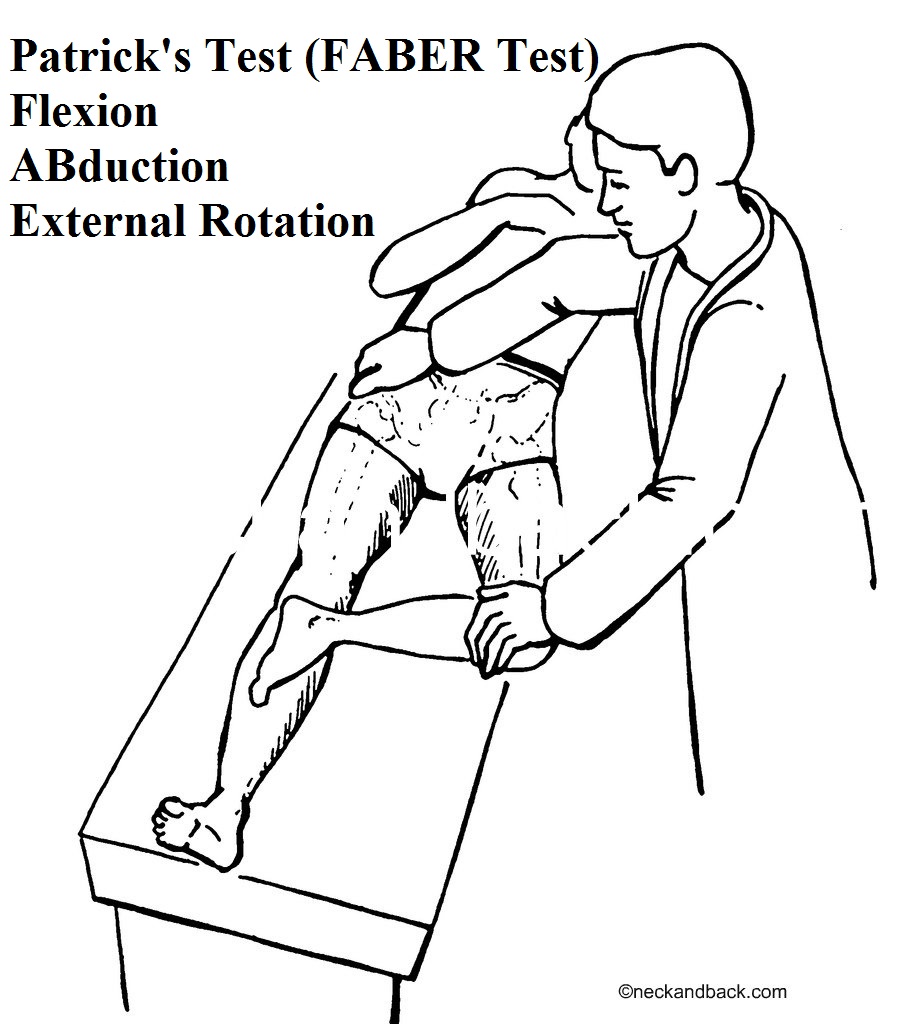
- Patrick’s test: Also known as FABER test, to test to sacroiliac joint inflammation
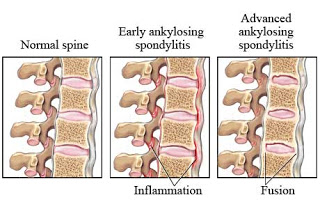
After exam, certain labs can be ordered to check for inflammation (ESR and CRP levels). An HLA-B27 can also be checked through blood work if there is a high suspicion for AS. However, imaging helps greatly in the diagnosis. X-rays can show changes in the SI joint and lumbar spine (such as Bamboo Spine). If it is early in the disease course, an MRI may be needed to catch subtle changes, such as erosions or inflammation.
How is it treated?

Treatment is aimed at maintaining mobility of the joints (especially the vertebrae), decreasing stiffness, and decreasing pain. Some modifiable risks include smoking cessation and increasing exercise. Home exercises and stretches can be beneficial, but a supervised physical therapy program usually provides greater benefit. Exercises usually focus on postural training, range of motion stretching, recreational activities, hydrotherapy, and local treatment with heat and cold.
When medications are decided on, Nonsteroidal anti-inflammatory drugs (NSAIDs) are usually first line therapy. Examples of NSAIDs includes:
- Ibuprofen (Advil, Motrin)
- Naproxen (Aleve)
- Meloxicam (Mobic)
- Celecoxib (Celebrex)
- Diclofenac (Voltaren)
- and others…
NSAIDs are used to decrease pain and inflammation, and hopefully aim to control back pain and stiffness.
However, it the inflammation and symptoms are not controlled, the next step in therapy is biologic medications. The main-stay is Anti-TNF biologics, which work by blocking TNF-alpha, an important component of the immune system which causes inflammation and ultimately leads to joint damage. Examples include:
- Adalimumab (Humira) – subcutaneous injection every 2 weeks
- Etanercept (Enbrel) – subcutaneous injection weekly
- Infliximab (Remicade) – IV infusion every 2 – 8 weeks
- Golimumab (Simponi) – subcutaneous injection monthly
- Certolizumab (Cimzia) – subcutaneous injection monthly
The newest FDA-approved medication for treatment is Secukinumab (Cosentyx), which works differently than the Anti- TNF medications. This medication inhibits an inflammatory protein known as IL-17, which is believed to play major role in other inflammatory diseases such as psoriatic arthritis, rheumatoid arthritis, and inflammatory bowel disease.
These medications are injectable or infusion based, and should be prescribed by a rheumatologist or trained physician. Steroids can be used, but show little long-term benefit. These medications all have possible side effects, and should be discussed with your rheumatologist prior to use.
Overall, if treated early and adequately, ankylosing spondylitis should not limit a patient’s daily life significantly, and patients can be expected to live a long, healthy life.
MORE SECTIONS on AS
What is Ankylosing Spondylitis?
Signs and Symptoms of Ankylosing Spondylitis
ALSO SEE
References
https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Spondyloarthritis
https://www.spondylitis.org/Ankylosing-Spondylitis
https://www.mayoclinic.org/diseases-conditions/ankylosing-spondylitis/symptoms-causes/syc-20354808






